Pilomatricoma
Background
Pilomatricomas (pilomatrixoma, calcifying epithelioma of Malherbe) are benign calcifying tumors that arise from skin appendages and are the most common solid cutaneous tumor in patients under 20 years of age. Imaging is generally not used in the evaluation of pilomatricomas, since they are usually superficial, small, and well-circumscribed. Pilomatricomas are slow-growing subcutaneous tumors that are usually less than 3 cm in diameter. The majority are found in the head and neck, followed by the upper extremities.Imaging
Radiographic features of pilomatricomas include regular contours, sharp demarcation from surrounding fat, and a normal overlying skin. Calcifications, when present, are usually speckled or sand-like, but can be large and dense in some cases.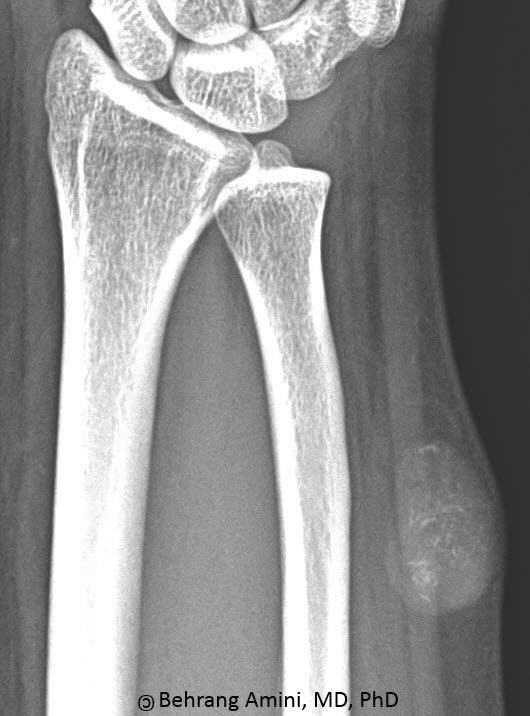
Frontal view of the distal forearm. Well-defined soft tissue mass with speckled calcifications.
Different ultrasound features have been described. Classically, these are hypoechoic solid nodules that are either fully or partially calcified. However, Pilomatricomas may also have internal fluid signal and a thick-wall.
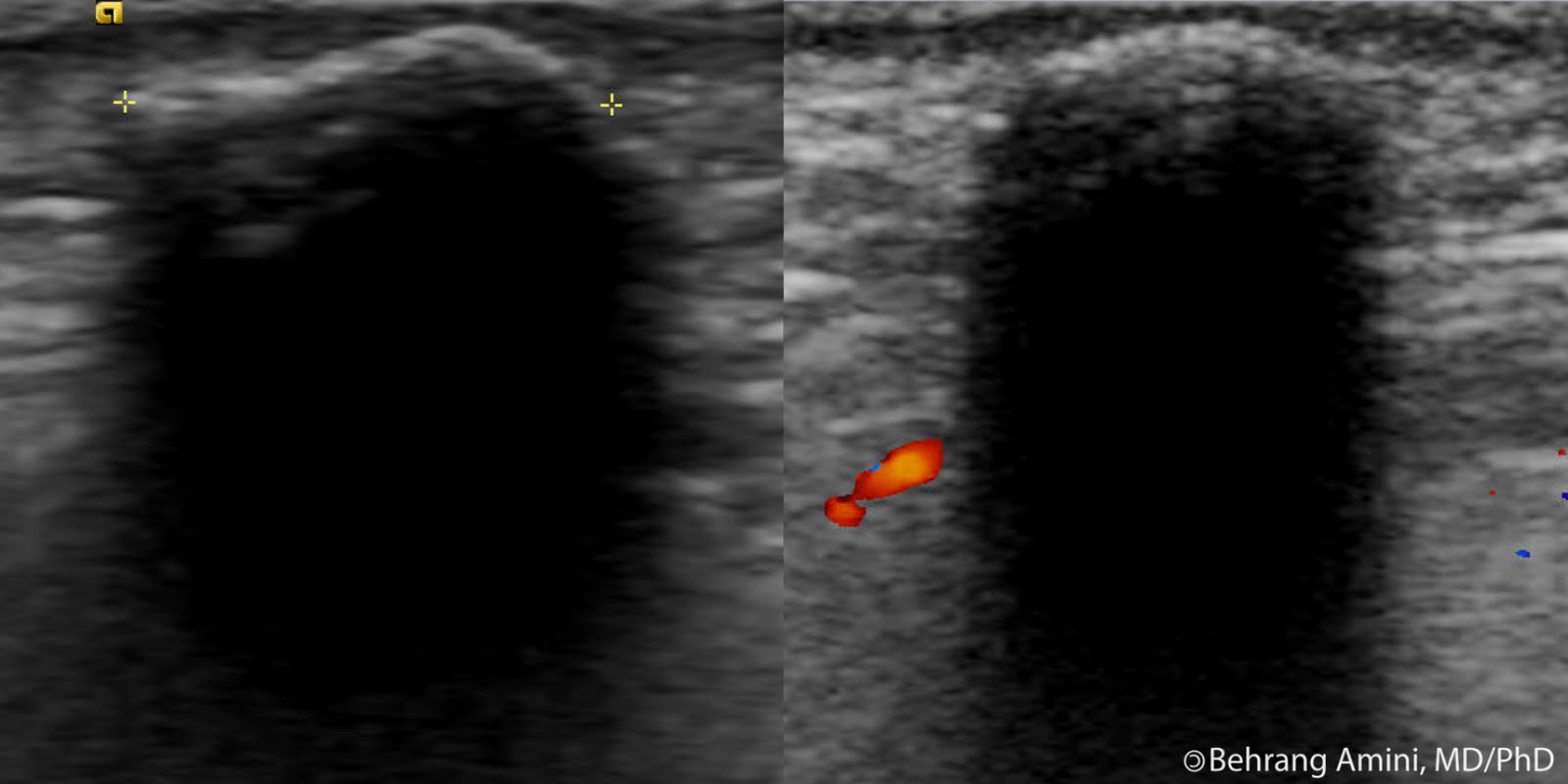
Ultrasound images of the elbow in a different patient. Echogenic superficial border with posterior shadowing due to calcifications.
MRI reveals a mass that is homogeneously isointense to muscle on T1-weighted images. Pilomatricomas can be hypointense to muscle on T2-weighted images with patchy hyperintense areas and striations that radiate from the center toward a hyperintense peripheral rim. Post-contrast images may reveal patchy or reticular enhancement centrally and peripheral enhancement of a connective tissue capsule. A case pilomatricoma without enhancement has also been reported. Peritumoral edema may be seen in some cases.
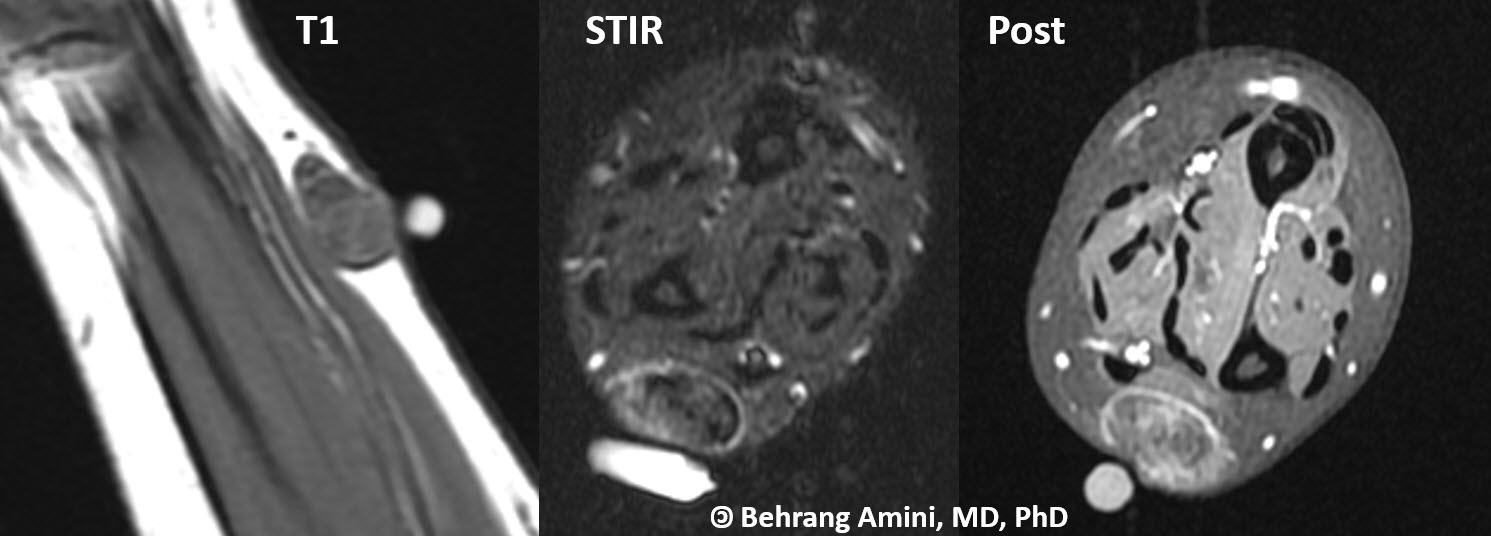
MR images of the distal forearm. Well-defined subcutaneous mass without muscle invasion. The mass has internal T1-hyperintense septae that have high T2 signal and enhance. Low-signal areas correspond to calcifications seen on conventional radiography.
Differential Diagnosis
- Hemangioma
- Calcifying hematoma
- Fat necrosis
- Parasitic infection
- Injection granuloma
- Calcinosis circumscripta
- Tumoral calcinosis
- Extraskeletal osteosarcoma
Treatment
Treatment is resection. Recurrence is rare.References
- De Beuckeleer LH, De Schepper AM, Neetens I. Magnetic resonance imaging of pilomatricoma. Eur Radiol. 1996;6(1):72-5.
- Gustin AF, Lee EY. Pilomatricoma in a pediatric patient. Pediatr Radiol. 2006 Oct;36(10):1113.
- Haller JO, Kassner G, Ostrowitz A, Kottmeler K, Perfschuk LP. Pilomatrixoma (calcifying epithelioma of Malherbe): radiographic features. Radiology. 1977 Apr;123(1):151-3.
- Hoffmann V, Roeren T, Moller P, Heuschen G. MR imaging of a pilomatrixoma. Pediatr Radiol. 1998 Apr;28(4):272.
- Lim HW, Im SA, Lim GY, Park HJ, Lee H, Sung MS, Kang BJ, Kim JY. Pilomatricomas in children: imaging characteristics with pathologic correlation. Pediatr Radiol. 2007 Jun;37(6):549-55.
- Solivetti FM, Elia F, Drusco A, Panetta C, Amantea A, Di Carlo A. Epithelioma of Malherbe: new ultrasound patterns. J Exp Clin Cancer Res. 2010 May 6;29(1):42.